Understanding
Cervical Cancer
Images do not represent real patients.
What is Cervical Cancer?
Cervical cancer is a type of cancer that starts in the cells of the cervix, which is the lower part of the uterus (or womb), that connects to the vagina. It happens when the cells in the cervix change in an unusual way and begin to grow out of control.1
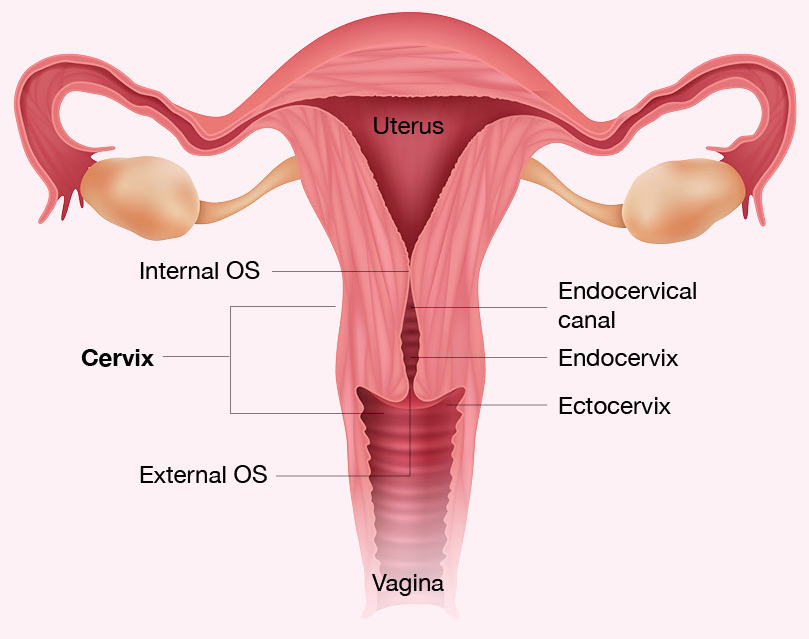
The cervix
The uterus (or womb), is where a baby grows and develops during pregnancy. The cervix is the narrow, lower end of the uterus that connects to the vagina.2
The cervix has 2 main parts:2
- Ectocervix: The outer, rounded part of the cervix, that connects to, and is visible from, the vagina. It has a small opening in the centre (called the external OS), that lets menstrual blood flow during periods.
- Endocervix: The inner part of the cervix, that forms a canal between the uterus (or womb) and the vagina. It connects to the uterus through another small opening called the inner OS.
The area where the two parts meet is called the transformation zone. Most cervical cancers start in this area.
Cervix Anatomy
Who is at risk?
A risk factor is something that makes it more likely for a person to develop a disease.2
HPV infection
Nearly all cervical cancers are linked to long-lasting infection with the Human Papillomavirus (HPV). HPV spreads through close intimate contact. Certain types of HPV — called high-risk types — can cause changes in the cells of the cervix. Most of the time, the body’s immune system clears HPV naturally, but if the virus stays in the body, it can cause long-term cell changes that may develop into cancer over many years. Many people may not even know that they have, or have had it.2

Family history of cervical cancer

Smoking

Long-term use of the contraceptive pill

A weakened immune system
Symptoms
Signs and symptoms of cervical cancer include:3

- Abnormal vaginal bleeding, such as bleeding after vaginal sex, bleeding after menopause, bleeding and spotting between periods, or having (menstrual) periods that are longer, or heavier than usual

- An unusual discharge from the vagina – the discharge may contain some blood and may occur between your periods, or after menopause

- Pain during sex
- Pain in the pelvic region
- Swelling of the legs

- Swelling of the legs
- Problems urinating or having a bowel movement
- Blood in the urine
These symptoms can also be caused by other conditions, not just cervical cancer. If you notice any of them, it is important to see your doctor.3
Types of Cervical Cancer
Cervical cancers are grouped by how the cells look under a microscope. The main types are called squamous cell carcinoma and adenocarcinoma:4
- Squamous cell carcinoma: This is the most common type, making up about 9 out of 10 cervical cancers. It starts in the flat cells of the outer cervix (exocervix), usually in the area where the outer and inner cervix meet (the transformation zone)
- Adenocarcinoma: This type develops from gland cells that produce mucus in the inner cervix (endocervix)
- Mixed types: Some cervical cancers have features of both squamous cell carcinoma and adenocarcinoma
Almost all cervical cancers are one of these two main types, but other rare types can also develop in the cervix.
Screening
The goal of screening for cervical cancer is to find cervical cell changes early, when treatment can prevent cervical cancer from developing. Sometimes, cancer is found during cervical screening. Cervical cancer found at an early stage is usually easier to treat. By the time symptoms appear, cervical cancer may have begun to spread, making treatment more difficult. The main ways to screen for cervical cancer include:4,5

HPV testing:
An HPV test looks for infection of high-risk types of HPV that can cause cervical cancer.

Pap smear testing:
A pap smear test can detect abnormal cells in the cervix before they become cancerous.

Images do not represent real patients.
When cervical cancer is caught early, treatment is more effective and successful. Regular screening can prevent cervical cancer and save lives.4 The best way for early detection, is to have regular screenings every 3 years.5,6
Stages of Cervical Cancer
A cancer stage describes the extent of cancer in the body, especially whether the cancer has spread from where it first formed, to other parts of the body. It is important to know the stage of cervical cancer, in order to plan the best treatment.10
Stage 1
The cancer has formed and is found in the cervix only.10
Stage 2
The cancer has spread to the upper parts of the vagina, or to the tissue around the uterus (or womb).10
Stage 3
The cancer has spread to the lower part of the vagina, which may include the wall of the pelvis. The cancer may also cause kidney problems and may involve the lymph nodes. Lymph nodes are small bean-shaped structures that are part of the immune system. Lymph nodes contain white blood cells that help the body fight infection and disease.10
Stage 4
The cancer is metastatic and has spread beyond the pelvis, or has spread to the lining of the bladder or rectum, or has spread to other parts of the body.2,10
Using Your Immune System to Fight Cancer with Immunotherapy
An important part of the immune system, is its ability to keep itself from attacking normal cells. To do this, it uses certain proteins on immune cells, called “checkpoints”, which act like switches that turn immune responses on or off. Cancer cells can sometimes use these proteins, to hide from the immune system.15
Immunotherapy are medicines that helps a person’s immune system fight cancer. By targeting the proteins on the immune cells, they can be used to treat cervical cancer.11,15
Follow-up Care During and After Treatment
As you go through treatment, you will have follow-up tests or check-ups. Some of the tests that were done to diagnose cervical cancer, or to find out the stage of the cancer, may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment, may be based on the results of these tests.11
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed, or if the cancer has recurred (come back).11
Use these visits as an opportunity for you to talk to your doctor about any symptoms, side effects, questions, or concerns that you may have.11

Images do not represent real patients.
Download materials
References: 1. National Cancer Institute. What is Cervical Cancer. 15 June 2023. Available from: https://www.cancer.gov/types/cervical. Accessed 24 September 2025. 2. National Comprehensive Cancer Network. NCCN Guidelines for Patients. Cervical Cancer. 2025. 3. American Cancer Society. Signs and symptoms of cervical cancer. 2 October 2024. Available from: https://www.cancer.org/cancer/types/cervical-cancer/detection-diagnosis-staging/signs-symptoms.html. Accessed 24 September 2025. 4. American Cancer Society. What is Cervical Cancer? 23 August 2023. Available from: https://www.cancer.org/cancer/types/cervical-cancer/about/what-is-cervical-cancer.html. Accessed 24 September 2025. 5. National Cancer Institute. Cervical Cancer Screening.
13 February 2025. Available from: https://www.cancer.gov/types/cervical/screening. Accessed 24 September 2025. 6. American Cancer Society. Can Cervical Cancer Be Found Early? Available from: https://www.cancer.org/cancer/types/cervical-cancer/detection-diagnosis-staging/detection.html. Accessed 24 September 2025. 7. American Cancer Society. Tests for Cervical Cancer 28 June 2024. Available from: https://www.cancer.org/cancer/types/cervical-cancer/detection-diagnosis-staging/how-diagnosed.html. Accessed 24 September 2025. 8. National Cancer Institute. Cervical Cancer Diagnosis. 01 March 2024. Available from: https://www.cancer.gov/types/cervical/diagnosis. Accessed 24 September 2025. 9. Johns Hopkins Medicine. Cervical Biopsy. Available from: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/cervical-biopsy. Accessed 24 September 2025. 10. National Cancer Institute. Cervical Cancer Stages. 16 May 2025. Available from: https://www.cancer.gov/types/cervical/stages. Accessed 24 September 2025. 11. National Cancer Institute. Cervical Cancer Treatment. 03 April 2025. Available from: https://www.cancer.gov/types/cervical/treatment. Accessed 24 September 2025. 12. National Cancer Institute. Types of Cancer Treatment. Available from: https://www.cancer.gov/about-cancer/treatment/types/surgery. Accessed 24 September 2025. 13. National Cancer Institute. Radiation Therapy to Treat Cancer. 15 May 2025. Available from: https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy. Accessed 24 September 2025. 14. American Cancer Society. Treating Cervical Cancer. Available from: https://www.cancer.org/cancer/types/cervical-cancer/treating.html. Accessed 24 September 2025. 15. American Cancer Society. Immunotherapy for Cervical Cancer. 01 July 2025. Available from: https://www.cancer.org/cancer/types/cervical-cancer/treating/immunotherapy.html. Accessed 24 September 2025.
ZA-NON-01074. Expiry date: 30/09/2027.





